In the context of injury or infection, the systemic immune system is rapidly deployed to the lung. Among the immigrating immune cells are bloodborne monocytes, which arrive in large numbers by day 3 after acute insult and establish a long-term presence in the tissue as monocyte-derived macrophages.
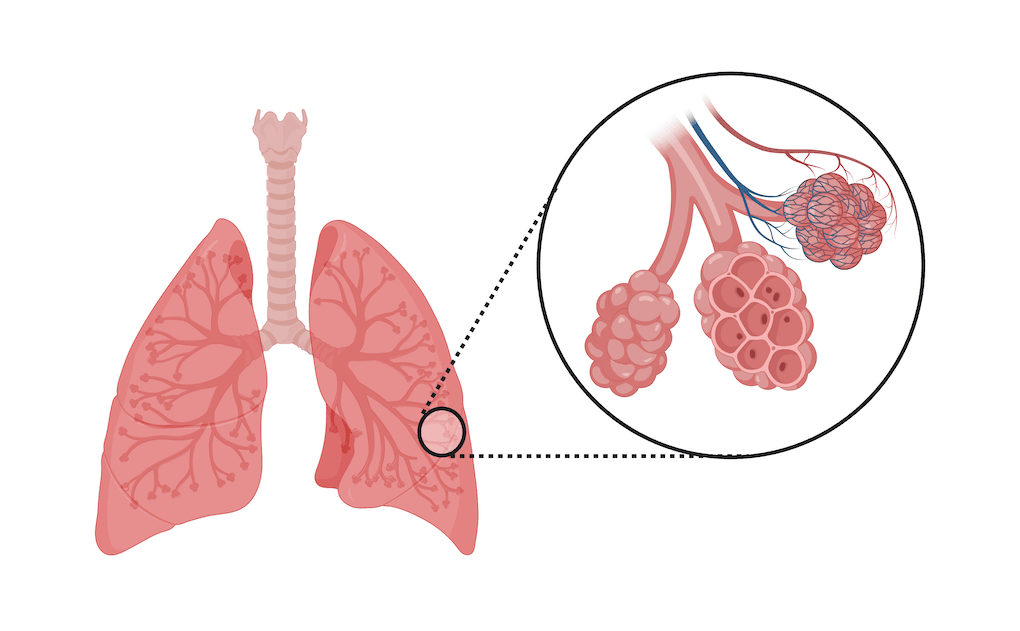
scRNAseq for macrophages in the early fibrotic period after lung injury showing alveolar (C1), monocyte-derived (C3), and transitional (C2) lung macrophages. From Aran et al, Nature Immunology 2019.
In the context of injury or infection, the systemic immune system is rapidly deployed to the lung. Among the immigrating immune cells are bloodborne monocytes, which arrive in large numbers by day 3 after acute insult and establish a long-term presence in the tissue as monocyte-derived macrophages.
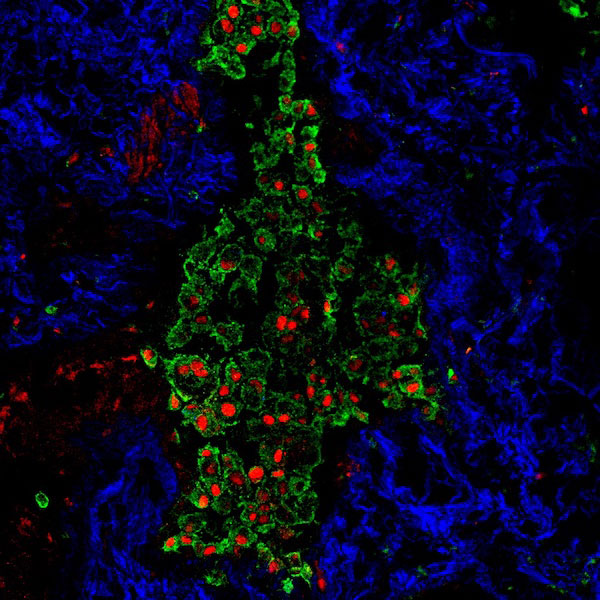
Macrophages marked by CD68 (green) bearing the monocytic marker MAFB (red) in an area of dense fibrosis visualized by second harmonic imaging (blue). From Aran et al, Nature Immunology 2019.
The Bhattacharya Lab at the UCSF Parnassus Campus is focused on the functional role of monocyte-derived macrophages in the onset and persistence of fibrosis in the lung. We are addressing the following major questions, with a goal of discovering new targets for therapy for acute lung injury and fibrosis:
-
What molecules released by monocyte-derived macrophages and other immune cells signal to and activate pro-fibrotic programs in parenchymal cell types such as fibroblasts and epithelial cells?
-
What reciprocal signals derive from these parenchymal cells to modify the immune response?
-
How can this pathologic crosstalk be reversed to combat fibrosis and restore lung health?
 University of California San Francisco
University of California San Francisco